HIV Patients in America’s Southern Cities Are Less Likely to be Virally Suppressed, Engaged in Care
Patients with HIV in Southern hospitals were less likely to be virally suppressed or engaged in care compared with patients from non-Southern hospitals, according to a new study by researchers at Columbia University’s Mailman School of Public Health. Most (80 percent) were on anti-retroviral therapy, 49 percent had a CD4+ cell count of less than 200 cells/µgL and 43 percent were virally suppressed. However, 13 percent reported not having had an HIV care visit within the past 12 months, compared with 8 percent of non-Southern patients. The findings are published online in Clinical Infectious Diseases.
“Few studies have examined regional differences in access to HIV-related care and outcomes,” said Morgan M. Philbin, PhD, assistant professor of Sociomedical Sciences at the Columbia’s Mailman School of Public Health. “The CDC has identified the South as the new epicenter of the HIV epidemic in the United States. Data suggest that Southern states tend to have lower rates of care linkage and engagement than those in the North or Midwest, and higher HIV-related mortality and poorer survival. Identifying geographic differences in treatment and care outcomes could assist policymakers in tailoring interventions, updating policies and determining areas of greatest need.”
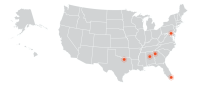
Philbin and colleagues, including Mailman School’s Lisa Rosen-Metsch, PhD, senior author, analyzed data from the National Institute on Drug Abuse Clinical Trials Network 0049 study, which took place between July 2012 and January 2014 and included 2,291 HIV-infected patients recruited from 11 hospitals across the U.S. that have a large number of HIV patients and a high prevalence of substance abuse among this population. The Southern hospitals were located in Atlanta; Baltimore; Birmingham; Dallas and Miami. The non-Southern sites included Boston, Chicago, Los Angeles, New York, Philadelphia and Pittsburgh. The analysis included private and public hospitals.
Of the 1,227 patients included in the analyses, 557 were hospitalized in Southern sites. Men made up over two-thirds of the participants. Approximately two-thirds (66 percent) of the participants were black, and the median age of the patients was 48 years.
Most participants reported an annual income of $20,000 or less, stable housing and health insurance. Just over half had ever used drugs, with 40 percent reporting having attended substance abuse treatment in the last year. A total of 88 percent reported having ever been in HIV care; 90 percent reported an HIV-related visit within the past year.
When Southern vs. non-Southern sites were compared, participants in the Southern sites were younger (46 years vs. 48 years) and more were black (71 percent vs. 63 percent), disabled (56 percent vs. 44 percent) or uninsured (24 percent vs. 17 percent). Patients in the South were less likely to report substance use (45 percent vs. 59 percent) or problematic drug or alcohol use (46 percent vs. 60 percent) or to have been treated for substance use (39 percent vs. 51 percent).
“Almost two-thirds of HIV-infected participants recruited from the Southern hospitals presented with a detectable viral load compared with half of participants in the non-Southern hospitals,” said Philbin. “While we cannot infer the reasons for this difference in viral suppression, the majority of participants were low-income ethnic/racial minorities who faced multiple health disparities, including unstable housing, food insecurity, unemployment, disability and education level. These problems may be particularly acute in Southern sites, where social safety net programs to address these issues may be especially underfunded or unavailable,” she noted. The findings “are consistent with other research that has shown HIV resources, Medicaid and social safety net programs that may benefit populations at high risk for HIV are generally underfunded in the South as compared to other parts of the U.S.”
Co-authors include Daniel Feaster, Lauren Gooden, Rui Duan, University of Miami Miller School of Medicine; Moupali Das, University of California San Francisco; Petra Jacobs, Raul Mandler, National Institute on Drug Abuse; Gregory Lucas, Johns Hopkins School of Medicine; D Scott Batey, University of Alabama; Ank Nijhawan, University of Texas Southwestern Medical Center; Jeffrey Jacobson, Temple University Lewis Katz School of Medicine; Eric Daar, Los Angeles Biomedical Research Institute, UCLA Medical Center; Deborah McMahon, Department of Medicine, University of Pittsburgh; Wendy Armstrong and Carlos del Rio, Emory University School of Medicine. The study was supported by the national Institute on Drug Abuse. See paper for list of grants and conflicts of interest statement.